COVID-19 patients show more signs of brain damage than Alzheimer’s sufferers
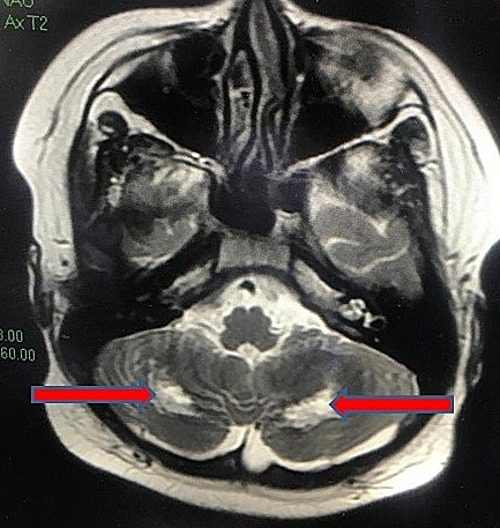
Patients hospitalized for COVID-19 had higher levels over the short term of blood proteins known to rise with neurological damage than non–COVID-19 patients diagnosed with Alzheimer’s disease, a new study finds.
Study authors found the markers for brain damage were even worse among patients that did not survive their coronavirus infection. Markers among patients who died from COVID were 124 percent higher than those who eventually left the hospital.
Serum neuronal, glial, and axonal neurodegenerative biomarkers, including t-tau, p-tau181, UCHL1, GFAP, and NfL were significantly elevated in patients with encephalopathy and worse discharge disposition after hospitalization for COVID-19. These markers correlated with the severity of COVID illness. Furthermore, levels of NfL, GFAP, and UCHL1 in hospitalized COVID patients were similar to, or higher than, levels observed in non-COVID AD dementia patients. Additional studies tracking trajectories of these biomarkers over time and their association with long-term cognitive outcomes among COVID-19 survivors are warranted.
Alzheimers Association Study – Comparison of serum neurodegenerative biomarkers among hospitalized COVID-19 patients versus non-COVID subjects with normal cognition, mild cognitive impairment, or Alzheimer’s dementia
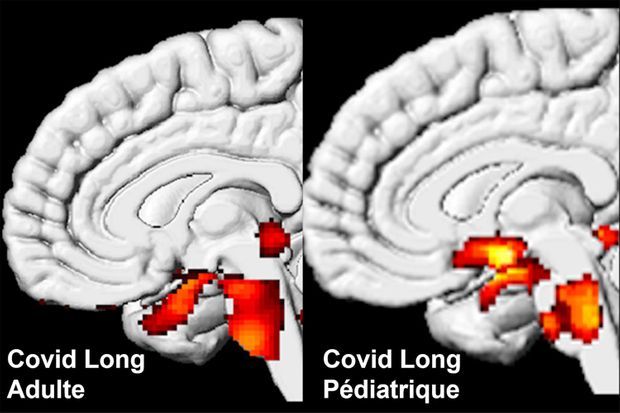
See also: January 2022 Preprint – Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain
So excited to be a part of this important study led by @michelle_monje on how significant longterm neurologic damage can occur after a mild respiratory-only SARS-CoV-2 infection. My own🧵on the findings of this study with relevance to #longCovid (1/)https://t.co/MgXZRrh899
— Prof. Akiko Iwasaki (@VirusesImmunity) January 16, 2022
Photo by jesse orrico on Unsplash